Abstract
The bone marrow (BM) is a dynamic stem cell microenvironment, harboring hematopoietic stem cells (HSCs) and various non-blood components such as endothelium, mural cells, multipotent stromal cells (MSCs) and their derivatives including osteoblasts, adipocytes, and fibroblasts. This stromal niche supports HSC-fate decisions and has been proposed as a major determinant of chemoresistance in hematological malignancies, such as acute myeloid leukemia (AML). Following chemotherapy, AML patients often suffer from relapse, in part due to chemoresistant leukemic stem cells (LSCs). There have been various indications in literature that leukemic cells remodel their niche, creating a permissive microenvironment for LSCs. However, which cell types respond and which underlying molecular mechanisms are involved skewing the compositional changes in the BM microenvironment remain unclear.
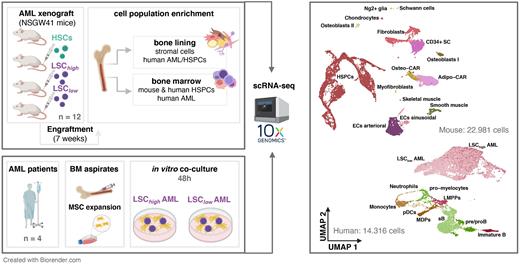
Here, we aim to investigate how high LSC frequency (LSChigh) versus low LSC frequency (LSClow) burden AML initiates BM niche remodeling in the favor of AML expansion, with a particular focus on the MSC lineages. We further aim to determine which stromal cell types interact with LSCs and how their composition is altered upon AML development. Additionally, we aim to visualize which cell types interact with and are positioned in close proximity to LSCs.
We combine single-cell transcriptomics of AML xenograft models and in vitro co-cultures of MSCs with primary AML. First, we set up clinically relevant murine xenograft models in which primary AML cells with either a low vs high LSC frequency (Garg et al., 2019) were injected in immune-deficient NSGW41 mice. As control, we injected cord blood-derived HSPCs. 6-7 weeks after engraftment, we harvested and digested the bones using our established protocol (adapted from Baccin et al., 2020) to recover the stromal cells with high efficiency. Besides, we also kept a femur per mouse for follow-up (multiplexed) immunofluorescence imaging. We enriched for human and mouse HSPCs, human AML cells, and mouse niche cells using FACS-based sorting, followed by scRNA-seq. Additionally, we isolated BM-derived mononuclear cells from healthy donors and AML patients and expanded the MSCs in vitro. We set up 4 independent co-cultures with MSCs and primary AML cells with LSChigh versus LSClow frequency. After 48 hours, we performed scRNA-seq to investigate transcriptomic changes and subsequent variant biological processes in the MSCs.
scRNA-seq profiling of the BM niche of our AML xenograft models demonstrates that AML presence significantly impacts the niche composition, leading to the expansion of Cxcl12-abundant-reticular adipocytes (adipo-CAR) and the decline of osteoblasts. When comparing LSChigh versus LSClow, we detect significant differences in abundance of certain stromal cells, including endothelium, adipo-CARs, and fibroblast subtypes. This suggests that the LSC-burden plays a critical role in the extent of niche remodeling. To further uncover the direct effects of LSCs on MSCs, we have established an AML-MSC co-culture system and perform scRNA-seq on the MSCs. In line with our in vivo data, we observe that cultured BM MSCs, especially upon exposure to LSChigh AML, suppress osteoblast lineage genes while overexpressing fibrosis-related genes. We are validating our observations using multiplexed immunofluorescence to further investigate the direct cell-cell communication of LSCs with their microenvironment.
Taken together, our data in murine AML models and human AML-MSC co-cultures unravel new insights into the BM stem cell niche composition and highlight a specific LSC-induced skewing of the mesenchymal lineage. Our data helps to better understand to which extent the BM microenvironment impacts AML disease progression and relapse due to residual LSCs.
Disclosures
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal